“We’ve had a support worker in our home 10 hours a day, helping us with meals. It’s more than we would have expected. Is this unusual?”
This message from Gemma, the mother of a 12-year-old with anorexia, made me gasp. How can any eating disorder service provide staff to spend all day in people’s homes?
This is so much more than what a mental health crisis outreach team typically provides.
If you’re a parent, I bet you wish you could have that level of help.
If you’re a clinician, you're probably wondering how a service like this could possibly work where you are. Surely you can’t afford it! Surely you don’t have the staff!
So here is the surprising information I collected from Gemma, the mother, and from Colette Storey, the service’s clinical lead.
Share this and let’s get more of this type of support around the world!
Gemma: “For us it was a lifeline. We embraced the help.”

"We were very scared that without the structure of the hospital, things would slip backwards and we could be re-admitted and back to square one, something that we wanted to avoid at all costs.
COAST being there from Day One saved us. They gave us the support; fed us the ropes to climb that Everest, and they pulled with us. They worked with us as a team to train us as parents to move forward meal by meal, day by day.
We made slow steps forward, and it was important to recognise it was literally hour by hour. Some days it was several steps back."
“They did not judge, they built a rapport with us and with our daughter and made it possible to get through each mealtime and each day.”
Surely this is a very expensive program?

“On the contrary,” says Colette. “Our pilot has produced huge cost savings”.
Did you say, savings?
"Yes, with this service, named COAST–ED (Community Outreach & Support Team for Eating Disorders), the correct word is ‘saving’:
“We have had estimated significant cost savings of £1.3 million in the first twelve months of the pilot and £2.7 million in the following ten months
COAST-ED is offered when a young person is likely to decline and need an inpatient mental health bed. And indeed, admissions have shrunk to zero, leading to big savings:
“I am pleased to say that there has not been a single admission to a mental health inpatient unit in over a year.”
That’s not just a cost saving. In a child’s life, that is of incalculable benefit. They might need a brief spell in a paediatric ward, but they won’t spend weeks or months in a psychiatric unit."
The bed days in paediatric wards have also shot down. For instance, where previously a child might have needed two weeks of refeeding in a ward, COAST can support a swifter discharge if they're medically stable.
More on the savings [click]
| SAVINGS | Apr 2023-Mar 2024 | Apr 2024-Jan 2025 |
|---|---|---|
| Mental health unit (SEDU or GAU) | £1,148,400 | £2,723,100 |
| Paediatric ward | £174,700 | £48,700 |
| Total | over £1.3 million | over £2.7 million |
The figures above represent the savings made (factoring in the cost of COAST), based on the assumption that all those receiving COAST's stream 1 or stream 2 intervention would have continue to decline and would eventually had to be admitted to a specialist eating disorder unit (SEDU) or a mental health general adolescent unit (GAU). Remember that none of the COAST youngsters needed admission.
For the paediatrics figures, the savings are estimated by comparing bed days before and after the COAST introduction.
That’s big savings! What is COAST-ED providing?
COAST provides a wrap-around layer of extra support for families who are getting a family-based treatment (FT-AN or FT-BN) and who need extra help. That could be because the child is very unwell, at risk of hospital admission, or stuck on certain aspects of recovery.
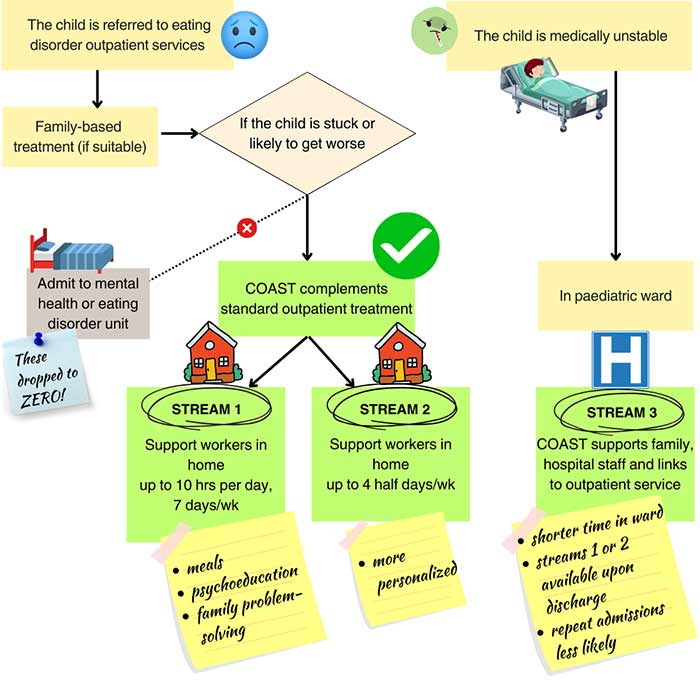

What Gemma received, with 10 hours of support a day, 7 days a week, is ‘Stream 1’ — the most intensive support.
It’s not just about getting the young person to eat. There’s also post-meal support, which includes psychoeducation for the young person, one-on-one. And twice a week another clinician visits to hold a family meeting."
More on Stream 1 [click]
"We offer up to 10 hours of support between 7:30am and 7:30pm, seven days a week.
We support the family during three meals and two snacks, and also gives post-meal support and psychoeducation. This is done by a Band 4 clinician who lives reasonably close.
We also provide a family meeting twice a week, based on systemic principles. The aim is to support the family in challenging the eating disorder and dealing with anything that is impeding progress. It’s done by a Band 6 clinician – i.e. a senior member of staff.
This is on a two-week reducing regime, with the hope at the end of two weeks, families may not need as much input from the COAST-ED.
We review weekly and can repeat the full support if needed.
Currently we repeat for a maximum of 3 cycles (6 weeks) before considering other interventions. There is also the option of being transferred to Stream 2.
Meanwhile the family is also under the care of the outpatient team, for evidence-based Anorexia or Bulimia Focused Family Therapy (FT-AN or FT-BN). And of course there is physical monitoring.
This FT team and the COAST-ED team meet regularly to share information. Indeed our COAST team members also work across other areas of the service. Some are part of reflective teams within FT-AN, or support the carers group or our paediatric clinic. Our senior practitioners also work to deliver FT-AN and1:1 therapy in the main service."
At the time of writing, COAST-ED is resourced to support up to 6 families at any one time, with no more than 2 in Stream 1.
More on the post-meal support and psychoeducation [click]
During the post meal support period, parents and the young person are offered psychoeducational modules.
For instance: ‘Understanding what it is like to have an eating disorder’ or ‘Distraction techniques’ or ‘What happens to the brain when starved’. It all depends on what is most useful to the family at any particular time.
We try and sense when is a good time for psychoeducation. When family members are overwhelmed, the team is very good at encouraging a game of UNO to lighten the mood!
"There’s also a Stream 2 – less intensive and more personalised version of Stream 1. That’s up to four half-day visits a week."
More on Stream 2 [click]
"Stream 2 aims to meet specific needs of the family and young person. There may bespecific goals, or preventative measures to stop further deteriroation.
For example, we might work on a particular struggle the family have in managing the ED. Or on a particular mealtime or snack."
With Stream 2, we visit families at home for up to four mornings or afternoons per week.
At the time of writing, COAST-ED is resourced to provide Stream 2 to up to 4 families.
"Finally there’s Stream 3 for youngsters in paediatric wards, to link them up with outpatient care."
More on Stream 3 [click]
"Stream 3 is for all youngsters admitted to a paediatric ward. It provides a smooth link with our community care (CYPEDS team – that's the outpatient service) and helps facilitate early discharge as soon as the child is medically stable. So what used to be two weeks of refeeding in the ward might now just be a few days.
Stream 3 is particularly useful where a young person became medically unstable and was hospitalised before being known to the outpatient service. In those urgent situations we offer assessments within 5 days (often much sooner), which means that families don’t have to wait to benefit from the eating disorder care pathway.
We also offer psychological support while the young person is inpatient, we assist our hospital colleagues, facilitate early discharge from the ward, and monitor any deterioration on discharge. And we activate more intense COAST input if needed."
Do COAST staff take over the meals at home?
“It’s about supporting and empowering the parents within the home and providing education.”
The staff don’t just feed your child. They help the parents learn how to help their child to eat. They support both parents and young person to reflect on what helps. On what might need to be different at the next meal, if last meal didn’t go to plan.
From Colette:
“It's been a huge reminder of what a difficult task families have in supporting their loved one. The skills are often counter-intuitive to the way people parent. Our job is not to shame or correct, but rather to help with new approaches that the evidence tells us work.”
More on what the support staff do [click]
Colette Storey told me: “Our aims with COAST were never to go in and ‘do to’ families. Whilst we actively take part in meal support, we are primarily there to support and empower parents or carers to challenge the eating disorder when it appears. We observe and review the skills and psychoeducation they need for their particular situation, in discussion with the family, the young person and the FT-AN team.
We are also in comamunication with senior practitioners and the FT-AN team about anything that may help with ongoing care. For example, if the eating disorder is doing lots of negotiating that is being accommodated."
What makes parents or carers succeed with meals? [click]
Colette told me: “We try to role-model that none of us is perfect. To pull from the work of Brené Brown, we assume everybody is doing the best they can, and approach the situation with kindness, compassion and empathy. This helps everyone to keep going through the difficulties again and again.”
This reminds me of a model used in Aachen, Germany, under psychiatrist Brigitte Dahmen. Germany tends to treat in inpatient units, so Aachen stands out in sending multidisciplinary teams to family homes. They too report big savings and treatment success.
You might wish staff to just feed your child, and that could indeed provide a kickstart to meal success, but ultimately, parents need to become competent, because their child is going to need help for quite a while.
I like how COAST saves parents from having to ‘reinvent the wheel’. When Family-Based Treatment (FBT) is applied zealously, a clinician may be so focused on empowering parents that they hold back from sharing any kind of tip. This makes us parents very cross, wastes precious time, and it’s why I wrote my book. Empowerment and competence require knowledge. Once we know what generally works, we can try it out, adapt it, and significantly reduce our floundering.
My own story is that our 10-year old spent a year in an inpatient unit, simply because we couldn't get her to eat at home. Even after discharge, meals could go either way. Our requests for coaching kept being declined ("We're not set up to do it"). Finally, our therapist came over for lunch. With just FOUR visits to our house, they made us super-competent, and from there on our daughter started to thrive. I reckon that if they'd started with home visits, the NHS would have saved a year of inpatient costs and dozens of outpatient therapy hours.
Gemma, how were things in hospital, before COAST?
"Our daughter spent two weeks in the local hospital’s paediatric ward, where she was on a re-feeding programme.
"As parents we felt all at sea. The thought of trying to successfully continue the re-feeding programme was more than daunting. It felt like we were about to climb Everest with no training and no equipment."
"Our experience in the hospital" [click]
"At first, we parents were not allowed in the room while the supervising nurse gave meals. Gradually, we transitioned to taking the lead. But we were still not at all confident that we could manage episodes of big emotions or lack of engagement. Our daughter was so out of kilter with her normal self. Connection at times was difficult: at times strained, or resistant and distant,or angry and confrontational, or tearful and emotional. It was hard to hit the right note as a parent. And even when we applied our very best selves and full empathy, sometimes a meal still did not work.
So we had immense anxiety about moving from the formal and structured hospital environment to our home.
This was on top of two weeks of little sleep, high emotion and complete disruption to family life. There were daily hospital visits for one parent, overnight stays for the other, juggling our business and life outside of her illness. The intense worry about our daughter's health left us barely able to cope."
"Our attempts to feed before the hospitalisation" [click]
"It was terrifying to imagine being back in the home situation we’d had before hospital, just two weeks before. Our daughter had been avoidant at mealtimes, feigning tiredness or illness, or pretending she had had such a “huge lunch” at school.
She’d been constantly exercising and restlessly moving around, not even able to sit and enjoy a film or family meal around the table. We were constantly scrambling to re-centre her and bring her back to herself and our normal family rhythm.
We had tried being strict, tried coaxing, tried having positive conversations outside of mealtimes. We knew things were getting worse and we were scrambling to make things right and help her.
By the time we had been admitted to hospital, she was barely drinking water, and we were in crisis. In hospital, the avoidance had been replaced with anger and utter despair, hatred and mistrust. So far away from the happy and bubbly girl she had been before slipping into the depths of the eating disorder."
Gemma, what was it like to have staff in your home all day?

"I cannot pretend having an additional person in the house was not tricky at times and left little room for privacy or completely relaxing, but these incredible people did their best to blend in with us, to help and support us and ultimately focus on the small steps to help our daughter back to a place of accepting food and helping meal times go well."
"I think it is important to recognise the reality – whilst we were so thankful for COAST being in our home and I honestly don’t think the outcomes would have been so positive for our daughter and us as a family without them – having new people, strangers in your home, with you for up to ten hours a day is a little daunting and takes a lot of adjustment.
However, given the circumstances of the eating disorder dominating the every day, we recognised we were in a completely new reality, so far removed from normal family life as we had known it. We wanted the help. We embraced the idea from the start, but I imagine this may not be the case for all; some families may find this level of support very intrusive.
But for us as parents, we understood this was a much- needed source of help and that it could be short term crisis management, it could be reviewed and changed as needed and we hoped it would help progress away from the critical place we were in."
Gemma: "We welcomed each member of the team”
"We made a plan with COAST so that our first support worker arrived ahead of our daughter arriving back from hospital with her dad, and I (mum) had time to show her around our home, get to know her a little and talk through strategies for re-settling at home and tackling meal times.
It was important to my husband and I that we welcomed each member of the team that joined us; we were trying to create harmony and balance and although not every day went well, we want to work as a team with our support worker and so tried to get to know them.
It was made clear that the support worker would bring their own packed lunches and meals, but because we knew they would be joining our daughter and us at the table for meals, we chose to cook the meal plan for everyone and invited them to eat the meals we were having, so we would all join in at the table together and make things feel as natural as possible. As a passionate cook this was my choice, but it certainly wasn’t expected.
What was lovely was that each member of the support staff embraced this and tried as much as possible to support us in the way we connect and work as a family. We felt their warmth and encouragement.
We did not have one person assigned, and so different support workers different days came to join us. Each had their own approach and style / a different connection with our daughter, some very young, some more mature as people, and so there were adaptations for the rhythm of the days. Some days went well. Some did not."
Gemma: “Our daughter did not want strangers in her home”
"Whilst we as parents wanted the support team in our home, it quickly became clear that our daughter did not.
Initially she tried to be nice, but on day one she quickly rejected the presence of the person supporting, clashed at the mealtime, then tried to run away. It took us over an hour to get her back into the house.
She did not want strangers in her home. She did not want to be observed at mealtimes. At this stage though she was very dominated by the eating disorder and they posed a threat to it winning."
Gemma: “Our daughter ended up looking forward to the workers she liked”
"Day by day, and with the change of support team on a sometimes daily basis, we found that some found a more natural rapport with her that she would accept and there were small break throughs.

One of the clever things was that each tried to find a way to that connection with her – and lots of distraction on the lead up to mealtimes.
One of the younger members of the team offered to do her nails. Another did artwork with her. Another more mature person brought fun board games and created a really lovely and relaxed bond with her. At mealtimes she would praise and say things were “good enough” when our daughter tried hard. I could tell she wanted to please her.
Others she clashed with, who were more strict about her leaving even the smallest amount of food on her plate did not get such a good reaction from our daughter and she resented their presence and intervention.
So some meals went well, and sometimes things were intense and distressing. She had preferences for some of the support team and in the end looked forward to seeing those she really liked. She would be very unhappy and surly and uncommunicative on other days with those she had decided she did not like or want around."
"Ultimately though I feel the blend of different people and approaches worked towards the eventual positive outcome."
Gemma: “Eva’s resources were invaluable too"
Note from Eva about blowing my own trumpet: Gemma messaged me, “Please do include the words I wrote about you, you were our original saviour and I so valued your emails on the way to hospital which helped me rationalise and put something in to context that at that stage I knew so little about. “ So here goes…
"It would have been harder, more intense and much longer to help our daughter to recover without your insightful resources, your emails about our specific situation, and the support we received in our home from COAST."
"COAST and the support they provided were invaluable in helping our daughter to recover. This was blended with family therapy and a parent group which gave tools to us as parents to understand some of the complex root causes of the eating disorder and possible ways to help recovery.
As parents, as soon as we realised our daughter was unwell, we went on a journey of discovery and learning. Before we even got to the hospital or knew COAST would be there to help us and that this service existed, we found your work, Eva through a friend’s recommendation.
I tried to download your book and when I couldn’t work out how to get this to work, I emailed and was amazed to get back an email from you, the author, a real person talking back to me and not just an automated message!

We began a dialogue in that early stage when we were desperately worried and unsure what to do and your wise and empathetic responses gave me so much context, when I was literally in freefall.
We were also clinging to the hope that our long-planned family trip could take place: to see my sister in Australia and our son, who we had not seen for 6 months. We were due to fly from the UK in 3 days time."
"It was absolutely the right decision not to get on a plane!!"
Click for more on that decision not to travel half way across the world
"I reached out to you as we were on our way to the hospital – for us as parents desperately hoping that they would say she should be OK. You emailed me straight back! I read your email on route – you were very realistic that this would not be a likely option and she would need help and a lot of time.
We were admitted to hospital that day, and in the end it was a relief to know we were in the right place and getting the help rather than on a plane.
We downloaded your audios and I begin listening to them in hospital, when we were apart from our daughter and it gave so much help and guidance in that early stage. We immersed ourselves in your words and perspectives and when we were introduced to COAST and parent group, they recommended and used your YouTube videos as part of their teaching.
Everything became very joined up and I just feel so grateful for all the wisdom and experience shared from you Eva, and the help and support from COAST which made it possible for us to begin to grasp the enormity of the eating disorder, and to start to find ways to help our daughter out of it.
She had closed down and was so very ill at this point that if we had not had that knowledge bank developing, and practical tools for working through mealtimes, it would have been very hard to create and develop the ways in which we could help and move forwards to starting a pathway to recovery.
I feel sure that without the book and audios by you, Eva, and the support provided by COAST and family therapy, our recovery would have been much slower at best, and at worst, peppered with relapses, re-admissions to hospital and desperate times for us as a family."
If you’re facing a similar dilemma to Gemma’s big Australia trip, you may be interested in my response [click]
Gemma, from everything I know, I would stay close to my home and the NHS. Motivation, things to look forward to, are usually very weak factors when the illness is at this strong stage which you describe. Refeeding is indeed a miserable affair for all, and it's your skills and determination, and energetic support from an ED team, that gets you safely through it, not attempts to cheer your girl up.
For instance, she wants so much to go, but she hasn't managed to eat that full-english breakfast, nor the lasagne for lunch or the pizza for dinner. Just sushi, which in her case is really a dieter's food. This indicates to me she's not close to managing based on motivation — and indeed I don't know anyone showing such strong signs of anorexia who is.
You could have a dangerous time on the long, tiring flight (even just standing in long queues could be a risk for her), with no medical rescue. If she's like many kids at this stage, she will eat almost nothing during the entire trip because of all the extra stressors. Then you could be in Australia with her eating very little and continuing to lose weight in spite of your lovely son's contribution — that's pretty likely. And then she's too unwell to fly home. She would probably need hospital in Australia, yet the best for her is a proper, systematic treatment delivered by an eating disorder service.
Indeed I'd say what you all need is to be taken in by eating disorder services locally and get the support you are entitled to in this country to beat this illness as energetically as possible. Rapid intervention will make your journey so much shorter and smoother.
Who is eligible for COAST, and is there much waiting?
Colette Storey told me, “We don't have a waiting list for COAST at the moment. I think this is because it sits within the main FT-AN outpatient community service: we are aware of young people who are deteriorating, and can step in quickly before they get worse.
At this point our criteria is that the young person has to be under our main service, have a diagnosis of AN/ BN/ OSFED and be on an family therapy (FT) pathway. The family also need to consent to the process.
We would like to roll out COAST to other areas of our service, such as those who are receiving individual support, have ARFID, or disordered eating or restrictive intake self-harm, (RISH).
This would need an adaptive version of what we have now, but we have ideas ready to go with this. For an adult population, we would also need adaptations. In all cases we want delivery to be in line with evidence-based practice.”
What skills and training are needed for COAST staff?
In other parts of the UK, there are intensive mental health teams that come to support meals in family homes for a few days. It can be fantastic, or parents may report that staff were not skilled and ‘said all the wrong things’. So what are the COAST staff like?
Colette Storey told me, "I once had a manager who told me, ‘You can learn a skill, but you can't learn passion.’ For me, one of the most crucial elements is having a genuine interest and a willingness to learn the specialty.”
Colette continued: “We are very committed to training individuals in the skills necessary to provide support in homes. But it also makes a big difference to that our team members are passionate about applying these skills.
Our senior members bring a wealth of therapeutic skills and extensive knowledge in the fields of eating disorders, paediatrics and general mental health. This is a formidable foundation for the families we support.
While staff have diverse roles, we value playfulness, kindness, compassion, and understanding for both the young person and their wider family.
When the service was set up, we did 2 weeks of induction training. It covered skills across the specialism and was delivered by all the disciplines within the team.
We have regular ‘reboot’ weeks where we continue professional development and reflect on recent cases.
We are hoping to put in live supervision to help deliver consistent care.
We utilise the sources available to us, such as the online BEAT training for healthcare professionals. We enable staff members to shadow other parts of the service.
We repeated our training this year and plan to do this annually. We also open this up to other services in the wider trust such as CAMHS and our colleagues in paediatrics."
How do you organise a team to spend so long in someone's home?
Colette wrote: “We cover all of Cornwall. Our staffing is spread across the whole county. We try to match families with staff who are close to them, to minimise travel. Although this is not always possible, staff will generally stay with one family for the whole shift which also helps with consistency."
Tips for other ED services to get the funding and approval

I asked Colette for tips that other eating disorder services might appreciate. She said, “Start with identifying the gaps in your own service. For us, it was to provide an alternative to admission to mental health units. Cornwall is a rural county and when someone is an inpatient, families have to travel extensive distances to visit.
When you identify the gaps, struggles and needs, you can get creative. You also need a put forward a solid business case for a pilot like this. And for that it’s important to have figure and outcome measures that reflect family experiences and clinical experience."
What and where is the COAST-ED service?
COAST-ED is a pilot project within the National Health Service (NHS) and is a branch of the Children and Young People with an Eating Disorder Service (CYPEDS) in Cornwall (UK). By April 2025, it will have been running for two years.
They have similar constraints to other NHS services, yet they’ve managed to do this pilot, and prove that it saves children from admission into a mental health unit, and saves a lot of money.
Colette Storey wrote:
“We are really proud of what it has become and how it wraps around the evidence-based treatment of our service.”
Quite so!
Gratitude to Colette and to Gemma for their generous time in writing this.
Parents and cliicians, please share! Somewhere, there will be another eating disorder service that will benefit from these ideas.
More on home treatment
It's rare to get professionals to help you all day long, as COAST does. Some form of support with meals at home is — or was — in place in other regions. For example, see this 2019 report from BEAT (in the UK): "Intensive day- and home-based treatment for eating disorders: an effective and less expensive alternative to inpatient care" (a short version is here).
My related post: * Professionals who help people with an eating disorder to eat at home *
Where to next?
Lots of compassionate and practical help from me. There's Bitesize, my searchable collection of short audios. My book is available in paperback or ebook. I can support you in individual video calls. And you can come to one of my online workshops — there's a topic for every stage of the journey.
This website is also full of tips. Use the search box, the keyword links, or pop over to the Frequently Asked Questions.




LEAVE A COMMENT (parents, use a nickname)